Past events at MIOT
MIOT performs a life-saving hybrid procedure, saving the life of a pregnant woman

Photographs Seen from Left to Right: Patient’s Husband, Mrs. Priyadharshini – Patient who underwent the procedure, Mrs. Mallika Mohandas, Chairman, MIOT International (Holding Patient Mrs. Priyadharshini’s baby), Dr. Saraswathy Gokulraj, HOD – Obstetrics & Gynaecology, MIOT International, Dr. Karthikeyan Damodharan, Director – Vascular & Interventional Radiology, MIOT International.
The 37-year-old Mrs. Priyadharshini embarked on her pregnancy, filled with anticipation and hope. It was an unplanned pregnancy, but she and her husband embraced the news with excitement, seeing it as a beautiful surprise.
At the twelfth week of her pregnancy in MIOT International, she was taken for a comprehensive ultrasound scan, offering a more detailed glimpse into her baby’s development. Simultaneously, a blood test for genetic screening was conducted to assess the baby’s health and identify any potential risks. With each passing day, Mrs. Priyadharshini and her husband diligently followed the doctor’s advice to ensure a healthy pregnancy.
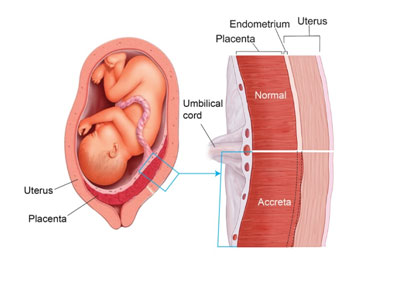
At the twenty-eighth week, through an ultrasonogram (USG) scan, medical experts at MIOT Hospitalsdiagnosed her with “Grade IV Placenta Previa with Focal Placenta Accreta”.
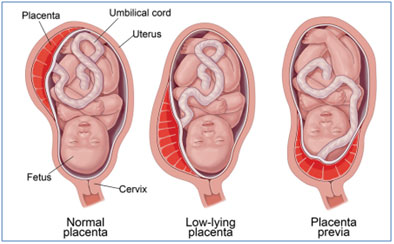
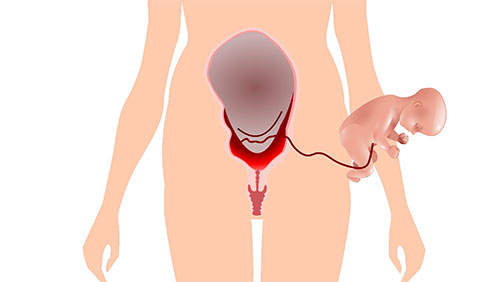
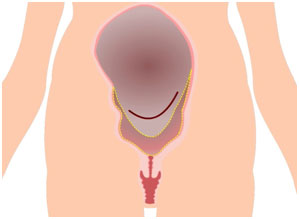
The Placenta provides oxygen and nutrients to the growing baby. It also removes waste products from the baby’s blood. The placenta attaches to the wall of the uterus, and the baby’s umbilical cord arises from it. Typically, during pregnancy, the placenta is primarily situated in the upper region of the uterus. This is very common in normal childbirth where the baby is delivered through the cervix.
Grade 4 Placenta Previa is a severe condition where the placenta is implanted very low in the uterus, completely covering the cervix making normal delivery impossible.
Common causes of Placenta Previa:
- Past history of surgeries involving the uterus
- Past history of uterine fibroids
- Family history – mother or sister having faced the same complication
What causes Placenta Accreta and who are at risk?
- Multiple C-sections: This results from scarring of your uterus from the procedures. The more cesarean sections a woman has over time, the higher her risk of placenta accreta.
- History of uterine surgeries: Patients who had fibroid removal, the scarring could lead to placenta accreta. Surgeries such as curettage (removing tissue from uterus) or endometrial ablation can also lead to scarring.
- Placenta previa: In people with placenta previa and a history of prior C-section deliveries, the risk for placenta accreta increases with the number of C-sections they’ve had.
- Have had more than one pregnancy.
- Are pregnant via IVF.
Risk to the mother:
- Damage to uterus and surrounding organs.
- Loss of fertility due to hysterectomy.
- Excessive bleeding that requires a blood transfusion.
- Blood clotting issues.
- Lung or kidney failure.
- Death.
Risk to the baby:
- Risk of intrauterine foetal death.
- Placenta accreta often leads to preterm birth. Preterm birth carries risks such as respiratory problems or trouble gaining weight.
Why is diagnosis of Placenta Previa and Placenta Accreta important?
For any pregnant mother with Grade 4 Placenta Previa with Placenta Accreta, as she approaches the delivery, the uterus will contract, and the baby’s head may impact the low-lying placenta and produce bleeding. If this bleeding becomes severe, it may result in intrauterine foetal death.
Also, to stop the torrential bleeding during delivery for patients with placenta previa and placenta accreta, immediate Hysterectomy (Uterus removal) is done to save the mother and child’s life. As a result of hysterectomy, the mother will not be able to get pregnant again. Also in cases with placenta accreta, the mortality rate can reach up to 7%.
To save the mother and child from such complications, these conditions have to be diagnosed during the scans especially in parents who are trying for their first child.
Approaching 30th week of pregnancy
As the weeks went by, and Mrs. Priyadharshini reached her 30th week of pregnancy, she started to experience bleeding. She was immediately rushed to MIOT Hospitals, where the medical team swiftly administered medications to control the bleeding.
If she had remained asymptomatic after the medication, the plan was for her to receive follow-up scans during her 32nd and 36th weeks. However, during her 33rd week of pregnancy, Mrs. Priyadharshini faced another episode of heavy bleeding that led to her immediate admission to the hospital. The medical team was fully prepared for her arrival, and were equipped to handle any potential complications. The dedicated medical team at MIOT Hospitals provided attentive care to Mrs. Priyadharshini for an additional two weeks, giving time for the baby to mature enough to be delivered without complications.
Typical approach by any Hospital:For high risk cases like Placenta previa with placenta accreta, more than 90% of hospitals, the recommended course of action for the mother’s safety is uterus removal. However, this approach can have profound consequences for the mother’s reproductive future.
Even in many advanced centres comprising the best team of doctors, they still lack the technology to handle such complex cases where the risk of radiation exposure is high, which can be hazardous to the developing baby.
Meticulous Planning by MIOT Experts
As her bleeding episodes persisted during the 35th week of her pregnancy, the team of doctors at MIOT Hospitals, who had meticulously planned for every possible scenario decided to take the next course of action. In Mrs. Priyadharshini’s case, the placenta fully obstructed the cervix, eliminating the possibility of a natural delivery. Therefore, the only viable option was a C-section. But traditional C-section procedure would inevitably lead to heavy blood loss from the placenta, endangering both mother and child. The risk was palpable, but the expertise at MIOT was unparalleled.
With Mrs. Priyadharshini’s and her baby’s safety as their top priority, MIOT’s Gynaecology and Interventional Radiology team devised a plan to first perform a pinhole procedure to stop the blood loss and then followed by a Lower (uterine) Segment Caesarean Section (LSCS).
How was the baby delivered?
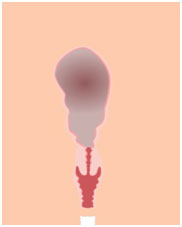
Mrs. Priyadharshini was taken to MIOT’s Biplane Cath Lab where two catheters were delicately inserted into her thighs, reaching the blood vessels that supplied nourishment to her uterus.
MIOT’s state-of-the-art Biplane Cathlab employs cutting-edge technology to minimize the use of contrast and radiation, safeguarding the baby’s developing kidney, skeletal, and nervous systems. Moreover, the Biplane Cathlab allows for the safe delivery of the placenta to save the mother’s life while preserving the integrity of her uterus. This ensures that both the mother and baby receive optimal care during medical procedures.
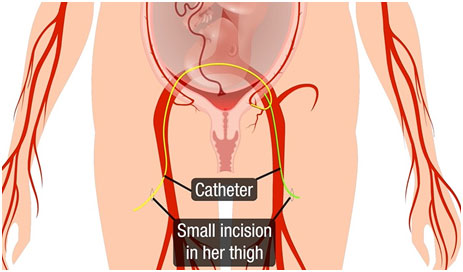
The balloons at the ends of the catheters were inflated within the arteries responsible for severe bleeding, blocking them without disrupting the overall blood supply to both the uterus and the baby.

The Gynaecologists then incised the uterus and opened up the placenta to deliver the baby.
Subsequently, the placenta was also removed as is usually done following the delivery of the baby. Once the placenta was removed, the inflated balloons were also shrunk.
Naturally, the uterus and the blood vessels shrink after the delivery which will stop further bleeding. But in Mrs. Priyadharshini’s case, despite the shrinking of her uterus and blood vessels, she was still bleeding.

MIOT doctors, already aware of such complications, were prepared to perform a follow-up procedure to stop the bleeding and save her life. MIOT doctors inflated the balloon once again and used the catheter, already in place in the uterine artery, to release temporary biodegradable particles which act as blocking agents to avoid excessive bleeding.
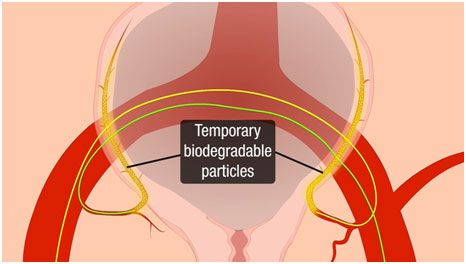
With the bleeding crisis receded, the catheter was gently removed, and the skilled MIOT experts carefully closed the uterus and abdomen.
Significance of a team comprising of Gynaecology & Obstetrics and Interventional Radiology:
The mortality rate in Placenta Previa with Placenta Accreta is up to 7%, making the joint efforts of Gynaecology & Obstetrics and Interventional Radiology team in such crucial moments even more essential, as it completely averted the mortality risk for both mother and baby.
By performing this hybrid procedure, MIOT Hospitals saved the lives of both the baby and the mother, eliminating the need for any blood transfusions (usually demands entire body’s blood volume) or removal of the uterus. This successful intervention not only averted life-threatening complications for the mother but also ensured a healthy recovery for both her and the baby, who was delivered safely and in good health.
MIOT’s Comprehensive Care
When it comes to the crucial moment of childbirth, individuals understandably seek out the finest hospitals and expert medical teams to ensure the safest delivery for both mother and baby. However, it’s important to note that even hospitals with renowned interventional radiology teams may sometimes lack the cutting-edge technology required to effectively manage exceptionally high-risk cases.
At MIOT, we offer not only a highly skilled medical team but also state-of-the-art medical technology tailored to address the unique challenges posed by such complex and high-risk pregnancies. We follow specialized protocols that have been developed to ensure the well-being and survival of both the mother and the baby.