Past events at MIOT
Free Cardiac Screening and Consultation Camp by MIOT at Port Blair
Mr. Vignesh, 32yrs old showed up at MIOT on 17th Feb, 2017 in a severely injured state after suffering a road traffic accident. Mr. Vignesh only son of the family, was brought up by his single mother. He was recently married and has a kid who is one and half years old. He owns a transportation company and lived a quiet and pleasant life.
On 13th Feb, 2017, around 10 in the night, Mr. Vignesh and his friend were returning back home on his bike after a movie. There was a large drainage hole dug on the road and mud stacked all along the hole. His friend, who was driving the bike, did not notice the stacked mud. The bike hit the stacked mud and Mr. Vignesh sitting in the back seat was thrown onto a concrete mixer machine. He was badly injured and immediately was taken to GB PANT Hospital, where he underwent initial management for 3 days.
There, they had identified severe chest injury and collection of blood in both his lungs. Tubes had to be placed on both sides of the lungs to drain the blood. For further management he was referred to MIOT Hospitals, Chennai under Anishi Scheme. He was airlifted along with a doctor from GB PANT, Port Blair to Chennai in a critical condition.
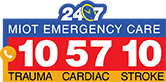
Emergency care at MIOT:
As soon as he arrived at MIOT, he was attended by the Critical Care Team. He was found to have difficulty in breathing and immediately needed ventilator for stabilization. On evaluation, he was found to have severe chest injury with multiple broken ribs on both sides, head injury, multiple fractured facial bones and eye injury. Most severely injured organ was the lungs with extensive collection of blood on both sides.
Note: A ventilator is a machine designed to move air into and out of the lungs, to provide breathing for a patient who is physically unable to breathe, or breathing insufficiently.
In most of the cases, the patient is removed from ventilator by 3rd or 4th day once the condition stabilizes, which was not possible for Mr. Vignesh. The lungs were still in a very bad state. On day 4, tracheostomy (A hole in the wind pipe) was done in view of him needing ventilator for a longer duration.
There was no improvement seen even by the 8th or 9th day. So, CT Chest was done, which showed damaged lungs with persistent blood collection. The Cardio-Thoracic team was called who took him up for “Decortication”, a Lung surgery performed to clean and remove all the collected blood and help in lung expansion.
Even a week post lung surgery by Day 15, there was no improvement. He continued to require high ventilator support for breathing. Repeat imaging was done which still revealed badly damaged lungs with presence of blood. He was taken up for repeat lung surgery on Day 16.
Even after all this efforts and surgeries, he was deteriorating. His oxygen levels in body were reducing and carbon-di-oxide levels were increasing. It was becoming difficult to sustain him on the ventilator. By day 18, on maximal ventilator support, blood pressure started falling and kidneys started shutting down. He had also picked up a bacterial infection in blood (Klebsiella) by this time. Over the next 12 hours there were dangerous levels of potassium and acidosis in his blood and it was getting tougher keeping him alive.
To stabilize kidney failure Continuous Renal Replacement Therapy (CRRT) was started. CRRT is a type of dialysis performed continuously that is used to treat critically ill, very unstable patients. Within the next 12hours, acidosis and potassium levels were brought under control.
By day 23 despite all these measures he crossed the maximal ventilator support possible and had progressed to multiple organs failure with dropping blood pressures and renal shutdown. This is when the doctors decided to take him to the next level of life support, the ECMO (Extra Corporeal Membrane Oxygenation).
ECMO
ECMO is a treatment used, when our lungs fail completely. It is a device that pumps blood through an artificial lung and back into the body. It’s done by inserting tubes into the neck vein and the leg vein. Blood drawn from one end goes through the machine, which adds oxygen and removes carbon-di-oxide. The re-oxygenated blood enters the body from other port. The purpose of ECMO is to provide oxygen, while allowing time for the lungs and heart to rest or heal.
Within 24hours on ECMO, things started changing. Mr. Vignesh oxygen levels had become normal. Blood pressure started stabilizing and was tolerating dialysis much better.
“The challenge is not putting a patient on ECMO, but it’s seeing him through” which can be done only by an expert team. The main problem associated with ECMO is bleeding from multiple sites; lungs, nose, mouth etc. This is because a drug called heparin needs to be administered, to prevent the blood from clotting inside the tubes and machine working. Handling this requires precision.
During the course of our ECMO we too had bleeding from multiple sites which were handled, however the worst episode was the lung bleed. It was the left lung bleed which had started pouring into the right lung. To protect the right lung from further damage the left lung had to be isolated. This bleeding had taken us back by few days in his lung recovery. Subsequently when bleeding stopped, the blood clots from the lungs were removed.
Mr. Vignesh kidneys continued to be supported with dialysis which by itself is a major challenge when on ECMO. He was not tolerating feeds and his nutrition had to be given through his veins.
Step-down from ECMO support to ventilator:
After 15 days on ECMO, with rest to lungs, his lungs had recovered reasonably well to remove from ECMO and step-down back to ventilator. By this time his blood pressures had stabilized and his kidneys had recovered to be off dialysis.
Day 40 in the ICU and 2 days after ECMO removal, he was found to have irregular heart rhythm. On evaluation with ECHO heart it was found that he had large fluid collected around his heart, known as pericardial effusion. He had to undergo emergency removal of about a litre of bloody fluid from around his heart in the Cath lab. The heart function had currently dipped to an extremely low level and his heart was hardly pumping. Medications were given to improve the heart function. The fluid taken from around the heart had evidence of bacterial infection.
With care, he continued to improve over time. Patients who are on bed for a very long time, one common issue, is pulmonary embolism. (Blood clots formed in the legs getting dislodged and reaching heart & lungs which can be catastrophic) At MIOT we anticipate such problems well in advance, placed a filter in the Inferior Venacava to trap these blood clots. Few days later he indeed did develop blood clots in his leg.
Breathing back to Normalcy:
After 49 days, Mr. Vignesh was completely freed from ventilator. He required a dedicated physiotherapy and rehabilitative team to work on his week hands and legs.
Discharged after 65 day:
After 60 days of ICU, he was shifted to ward. He was able to stand, walk and started taking normal food. He got discharged by the 65th day.
2 weeks later he came for a review. His Chest X-ray was totally clear and ECHO showed regained heart function. The past was history. He was back to his family and little daughter.
Conclusion:
ECMO is reliable and important treatment in patients with failing lungs or failing heart. ECMO comes with unique challenges which require expertise, and a huge team effort & infrastructure to run successfully. So being at the right place at the right time becomes very crucial.
Team Effort:
“Talent wins games, but teamwork wins championships”, a very famous saying by Michael Jordan best suits our team of doctors at MIOT. It was not the effort of 1 doctor, but an umbrella of doctors and their teams starting from Critical care, Cardio thoracic, Trauma, Neuro surgery, Nephrology, Pulmonology, Radiology, Blood bank and Microbiology. But not to forget our nurses and the Physiotherapist who worked hand in hand to make the impossible, possible today.
Adding on to all the effort put by doctors, the positive attitude of Mr. Vignesh’s mother and her sheer determination to see her son alive again stood as a major pillar of strength. When people lost hope, she fought along with Mr. Vignesh, and stood by the stance “A mother can never be replaced in anyone’s life”.